Incoming: Avian Flu EUA Tests + mRNA Injections
Staging a pandemic based on a whopping TEN case "public health emergency"(just in time for the election)
Slide over Assassin Theatre, it’s the Pandemic-thon Sequel Event we’ve all been waiting for…
Bird Flu. Or Highly Pathogenic Avian Influenza. Actually any Influenza A Virus.
How To Stage a Pandemic
* See more about faking pandemics here and here
1. Declare a Public Health Emergency ✅
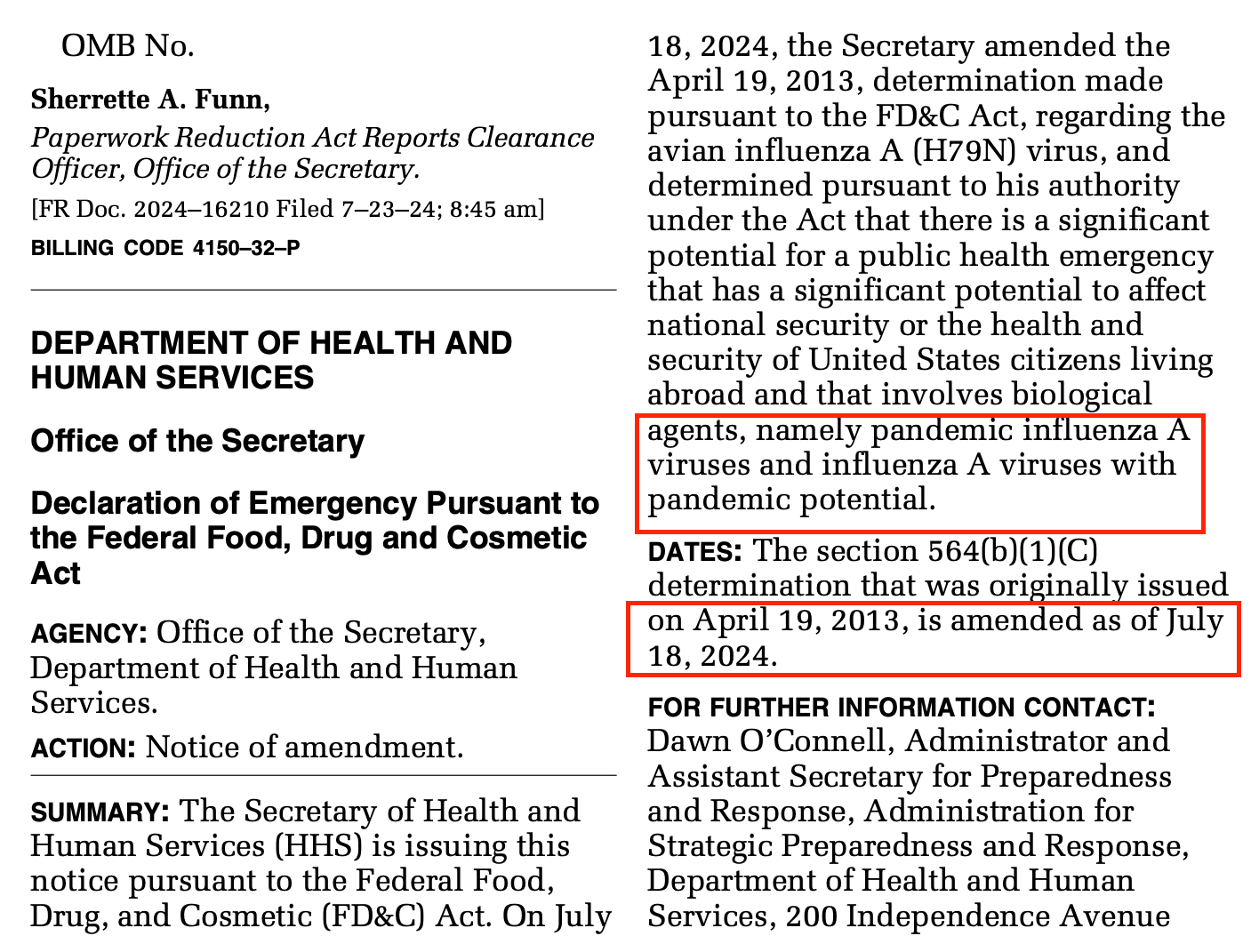
Broadening the April 19, 2013, determination to apply to pandemic influenza A viruses and influenza A viruses with pandemic potential—rather than just H7N9 specifically—would appropriately cover the range of known and emerging influenza A viruses that present a significant potential for a public health emergency. Therefore, I have now amended the April 19, 2013, determination to recognize that there is a significant potential for a public health emergency that has a significant potential to affect national security or the health and security of United States citizens living abroad and that involves biological agents, namely pandemic influenza A viruses and influenza A viruses with pandemic potential.
2. Emergency Use Authorization for Testing ✅
Testing is the lynchpin. Testing is the lynchpin. Testing is the lynchpin.
Please recall Covid and the abundant and asymptomatic testing. Based on “genetic sequences” from a computer. Remember all of those convenient drive through testing places? Remember the tests that got freely delivered to your home? Remember the free tests provided to schools? Those tests that told people not experiencing symptoms that they were “sick”. The “pandemic” could have never been staged without the testing.
According to the CDC, the old Influenza A tests won’t work for this new avian flu. Sounds like a job for an EUA test!
From CDC:
Existing, commercially available FDA-cleared molecular assays [e.g., Real-Time RT-PCR (rRT-PCR)] may fail to detect novel influenza A viruses or may detect with results that indicate "influenza A positive", but with subtype not identified. For these assays a novel influenza A virus may give an influenza A "unsubtypeable" result. Clinicians and laboratorians using molecular assays that can detect all currently circulating influenza A virus subtypes (i.e., "seasonal influenza" subtypes) who identify an unsubtypeable result should contact CDC and their state or local public health laboratory for additional testing (see below).
Rapid influenza diagnostic tests (RIDTs) and immunofluorescence assays are antigen detection tests that only identify whether an influenza A virus is detected and have unknown sensitivity and specificity to detect human infection with novel influenza A viruses in respiratory specimens. Some studies suggest that antigen detection tests have low sensitivity to detect HPAI A(H5N1) viruses. Therefore, negative results from either type of test do not exclude novel influenza A virus infection, especially in patients with signs and symptoms suggestive of influenza. A negative test result could be a false negative and should not be used as a final diagnostic test for influenza, including novel influenza A virus infection. These tests may yield a positive influenza A result for a specimen containing novel influenza A virus but cannot identify the subtype and cannot distinguish novel influenza A virus from seasonal influenza A virus infection. Therefore, testing by rRT-PCR is recommended at state health laboratories for any patient with suspected novel influenza A virus infection.
Fear not! Alveo Technologies is on the case!
Rapid test for bird flu developed
By News Desk on July 22, 2024
A rapid Avian influenza molecular test, detecting the latest H5N1 variants in cattle and the recent human inflections in Colorado, is now available to fight bird flu.
The rapid test is the latest scientific advancement against bird flu and comes from Alveo Technologies Inc., a leader in molecular sensing and diagnostics with a proprietary technology platform. The test is not yet out. Alveo expects to begin shipping an avian flu test for poultry this quarter to the EU and Middle East. As for cattle and humans, Alveo has shown via computer simulations that their test should detect the viruses found in recent Colorado infections. Alveo is working on development of a test for cattle and humans,
Alveo has announced that it has demonstrated in silico
(pssst, Sarah here…”in silico” means modeling IN A COMPUTER)
that its rapid, handheld, point-of-need molecular diagnostic for avian influenza can detect the H5N1 variant based on sequences published from recent human infections in Colorado and those found in infected cattle.
Alveo expects the Flockscreen LAMP Avian Influenza Molecular Test for poultry, the first diagnostic of its kind to test both cloacal and oropharyngeal samples and which the company developed with numerous partners, to begin shipping to Europe and the Middle East in the third quarter of 2024 once validation and verification activities have concluded with the relevant regulatory bodies. The company is now working to validate avian influenza diagnostics for human and bovine use cases.
Alveo’s rapid detection platform provides real-time data and empowers more industries to Know Sooner, Act Faster™.
Are you wondering how many cases of this avian influenza warranted a Public Health Emergency?
Ten.
Gosh, I hope those assholes hop on locking us down before it really gets out of control. And especially before November. It would be a shame not to inject some contention into an already volatile situation.
CDC A(H5N1) Bird Flu Response Update, July 19, 2024
CDC Update
July 19, 2024 – CDC continues to respond to the public health challenge posed by a multistate outbreak of avian influenza A(H5N1) virus, or “H5N1 bird flu,” in dairy cows, poultry and other animals in the United States. CDC is working in collaboration with the U.S. Department of Agriculture (USDA), the Food and Drug Administration (FDA), Administration for Strategic Preparedness and Response (ASPR), state public health and animal health officials, and other partners using a One Health approach. Since April 2024, 10 human cases of avian influenza A(H5) infection have been reported in the United States. Four of these cases were associated with exposure to sick dairy cows and six were associated with exposure to avian influenza A(H5N1)-infected poultry.* [A][B] This includes two additional cases in Colorado that were confirmed by CDC this week and not previously reported. The two new cases were in poultry workers with exposure to infected poultry during depopulation and disposal activities. Similar to previous cases, illness was mild. Based on the information available at this time, CDC’s current H5N1 bird flu human health risk assessment for the U.S. general public remains low.
Okie dokie, y’all…you know what’s next, right?
3. Untested Medical Countermeasure Deployment
Penn Researchers Develop Experimental mRNA Avian Flu Vaccine
Promising preclinical results suggest mRNA vaccine platform could limit the impact of avian flu pandemics
May 23, 2024
PHILADELPHIA— An experimental mRNA vaccine against avian influenza virus H5N1 is highly effective in preventing severe illness and death in preclinical models. The vaccine could potentially help manage the outbreak of the H5N1 virus currently circulating in birds and cattle in the United States, and prevent human infections with the virus, according to research from the Perelman School of Medicine at the University of Pennsylvania, published today in Nature Communications.
“The mRNA technology allows us to be much more agile in developing vaccines; we can start creating a mRNA vaccine within hours of sequencing a new viral strain with pandemic potential,” said Scott Hensley, PhD, a professor of Microbiology at the Perelman School of Medicine. “During previous influenza pandemics, like the 2009 H1N1 pandemic, vaccines were difficult to manufacture and did not become available until after the initial pandemic waves subsided.”
Hensley and his laboratory collaborated in the study with the laboratory of mRNA vaccine pioneer and Nobel Prize winner, Drew Weissman, MD, PhD, the Roberts Family Professor in Vaccine Research and Director of Vaccine Research at Penn Medicine.
“Before 2020, experts thought the influenza virus posed the greatest risk of causing a pandemic, and we had limited options for creating a vaccine if that had happened,” said Weissman. “COVID-19 showed us the power of mRNA-based vaccines as tool to protect humans from emerging viruses quickly, and we are better prepared now to respond to a variety of viruses with pandemic potential, including influenza”
Most influenza vaccines are egg-based, where experts inject fertilized chicken eggs with what they predict will be the dominant viral strain, let it replicate, and then inactivate the virus to use in the flu shots distributed globally. However, viruses must first be adapted to replicate in fertilized eggs before these conventional vaccines can be produced, which can take up to six months, presenting potential problems for quickly producing vaccine when it’s needed most during the first few months of a pandemic. mRNA vaccines are easily and quickly adapted to protect against different strains of influenza viruses, and don’t require eggs for their development.
The Penn researchers developed an mRNA vaccine targeting a specific subtype of the H5N1 virus that is circulating widely in birds and cattle. While it rarely infects humans, some fear that the virus may evolve and cause a human pandemic. The researchers found that the vaccine elicited a strong antibody and T cell response in mice and ferrets. What’s more, the animals maintained high levels of antibodies even a year after vaccination. Additionally, the researchers found that vaccinated animals who were subsequently infected with H5N1 cleared the virus more rapidly and displayed fewer symptoms than unvaccinated controls. The researchers also note that all of the vaccinated animals survived following H5N1 infection, whereas all the unvaccinated animals died.
Finally, researchers compared the mRNA vaccine response in mice to their response to a traditional egg-based vaccine and found that the mRNA vaccine was just as effective; both vaccines elicited strong antibody responses, regardless of prior seasonal flu exposures.
This research was funded by the National Institute of Allergy and Infectious Diseases, National Institutes of Health, and the Department of Health and Human Services (75N93021C00015, 75N93021C00016, R01AI08686, and R01AI126899).
For more research on the groundbreaking mRNA research at Penn Medicine, visit: https://www.pennmedicine.org/mrna.
Editor’s Note: Scott Hensley and Drew Weissman are co-inventors on patents that describe the use of nucleoside-modified mRNA as a platform to deliver therapeutic proteins and as a vaccine platform. Hensley also receives consulting fees from Sanofi, Pfizer, Lumen, Novavax, and Merck.
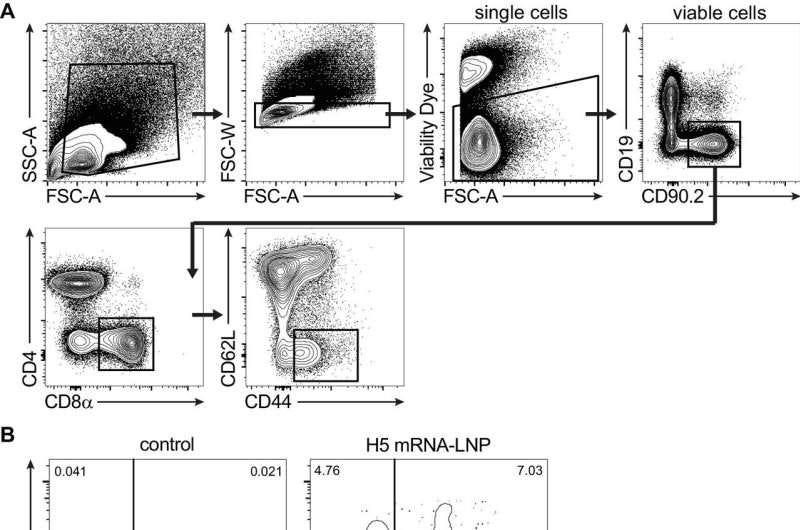
Here’s a picture from their study:
Would you believe that mRNA shills Scott Hensley and Drew Weissman aren’t the only ones working on lining their pockets while murdering the world developing life saving vaccines:
New initiative launched to advance mRNA vaccine development against human avian influenza (H5N1)
29 July 2024
Geneva, Switzerland
A new project aiming to accelerate the development and accessibility of human avian influenza (H5N1) messenger RNA (mRNA) vaccine candidates for manufacturers in low- and middle-income countries has been launched today. The Argentinian manufacturer Sinergium Biotech will lead this effort leveraging the World Health Organization (WHO) and the Medicines Patent Pool (MPP) mRNA Technology Transfer Programme.
The mRNA Technology Transfer Programme, jointly developed by WHO and MPP, was launched in July 2021 with the aim to build capacity in low- and middle-income countries (LMICs) for the development and production of mRNA-based vaccines. Sinergium Biotech, a partner in the mRNA Technology Transfer Programme, has developed candidate H5N1 vaccines and aims to establish proof-of-concept in preclinical models. Once the preclinical data package is concluded, the technology, materials, and expertise will be shared with other manufacturing partners, aiding the acceleration of the development of H5N1 vaccine candidates, and bolstering pandemic preparedness efforts.
Since its inception, the mRNA Technology Transfer Programme has developed and implemented a platform that was used to establish the immunogenicity, efficacy, and safety of a COVID-19 vaccine candidate in preclinical animal models. Afrigen is the centre where the platform was created and is being validated and this technology is now being transferred to manufacturing partners to adapt and enhance it for other critical disease targets. The progress made by the mRNA Technology Transfer Programme is a vital part of WHO and MPP’s efforts to improve the availability, access, and use of mRNA vaccines for better vaccine equity globally.
Yeah…it’s happening.
Of relevant interest:
Please see Katherine’s work for more information on the legal framework that allows for the staging of pandemics and the deployment of bioweapons labeled as medical countermeasures within the “boundaries” of the law:










When they allegedly infected those ferrets which had been transfected by these mRNA injections that are designed to injure & kill recipients (ferret or human), where dod they get the birdy flu “virus” from?
No one has such a thing, because it doesn’t exist.
Perhaps they rubbed a suspected infected birdy up against the ferret?
I've never been tested or vaccinated, but I just commented on one of Sage's posts about how many people I deal with in my daily life who are testing and talking about "COVID going around." People are idiots.