Ozempic and GLP-1s FOR OBESITY To Be Covered By Medicare & Medicaid
Proposed Rule posted 12/10/2024 on the Federal Register
In a continued effort to make sure that everyone takes as many injections as possible, the Federal Register was updated with a proposed rule today. Of course all the vaccines are mentioned (which I’ll address separately) but a stand out addition is GLP-1 drugs like Ozempic for treatment of OBESITY (absent of a comorbid condition) and overweight as long as you have a comorbidity (for now) ← CMS is inviting you to please submit comments suggesting that overweight be recognized as a disease too.
Medicare and Medicaid Programs; Contract Year 2026 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly
A Proposed Rule by the Centers for Medicare & Medicaid Services on 12/10/2024
👉 AOM = Anti-Obesity Medications
In the spirit of the depopulation agenda equity, inclusion, and health, we need to reinterpret a statute:
Given the prevalence and the impact of obesity in the U.S., the Biden-Harris Administration released the National Strategy on Hunger, Nutrition, and Health focused on ending hunger and reducing diet-related diseases such as obesity.[] One of the Strategy's pillars is integrating nutrition and health, which recognizes the opportunities within Medicare and Medicaid to support beneficiaries' access to nutritious foods, obesity counseling, and other nutrition-related services. Reinterpreting the statute to provide for coverage for AOMs for individuals who have obesity would build on that National Strategy by offering another tool that can support Medicare and Medicaid beneficiaries in addressing obesity and living healthier lives.
Because disparity you assholes!
Further, CMS believes that excluding AOMs from Part D coverage has created a scenario where Medicare Part D enrollees with obesity have been unable to access drug therapy to treat what is recognized as a chronic disease, potentially exacerbating health disparities in groups disproportionately affected by obesity.
As I understand it, this proposal suggests that people who are obese, that do not have another condition for which a GLP-1 drug would be indicated (like Type 2 Diabetes), don’t have access to these amazing injections.
And that sucks for them.
Because who wants to address those issues with bullshit like diet and exercise?!?
4. Part D Coverage of Anti-Obesity Medications (§ 423.100) and Application to the Medicaid Program
We are proposing to reinterpret the statutory exclusion of agents when used for weight loss to allow Part D coverage of AOMs when used to treat obesity by reducing excess body weight or maintaining weight reduction long-term for individuals with obesity who do not have another condition for which the prescribed use is an MAI that is covered under the current Part D policy. The proposed reinterpretation would also apply to the Medicaid program. Thus, AOMs could not be excluded from Medicaid coverage under this interpretation when used for weight loss or chronic weight management for the treatment of obesity. Coverage of AOMs and drugs that contain the same active ingredient as AOMs that meet the definition of a covered outpatient drug are already subject to section 1927 requirements when used for an indication, other than weight loss, that is an MAI, and Medicaid must cover those products when they are medically necessary. Under our proposed reinterpretation, AOMs approved for weight loss and chronic weight management that are used for weight loss in individuals who do not have obesity or another condition that is an MAI for the AOM would remain excluded from the definition of covered Part D drug and would remain optional benefit for Medicaid programs.
Now that obesity is considered a disease, these injectable products should be available for obese people that need to lose weight, regardless of whether or not they have comorbidities. Stop discriminating. It’s a disease and it needs medicine. STAT.
2. Proposed Reinterpretation
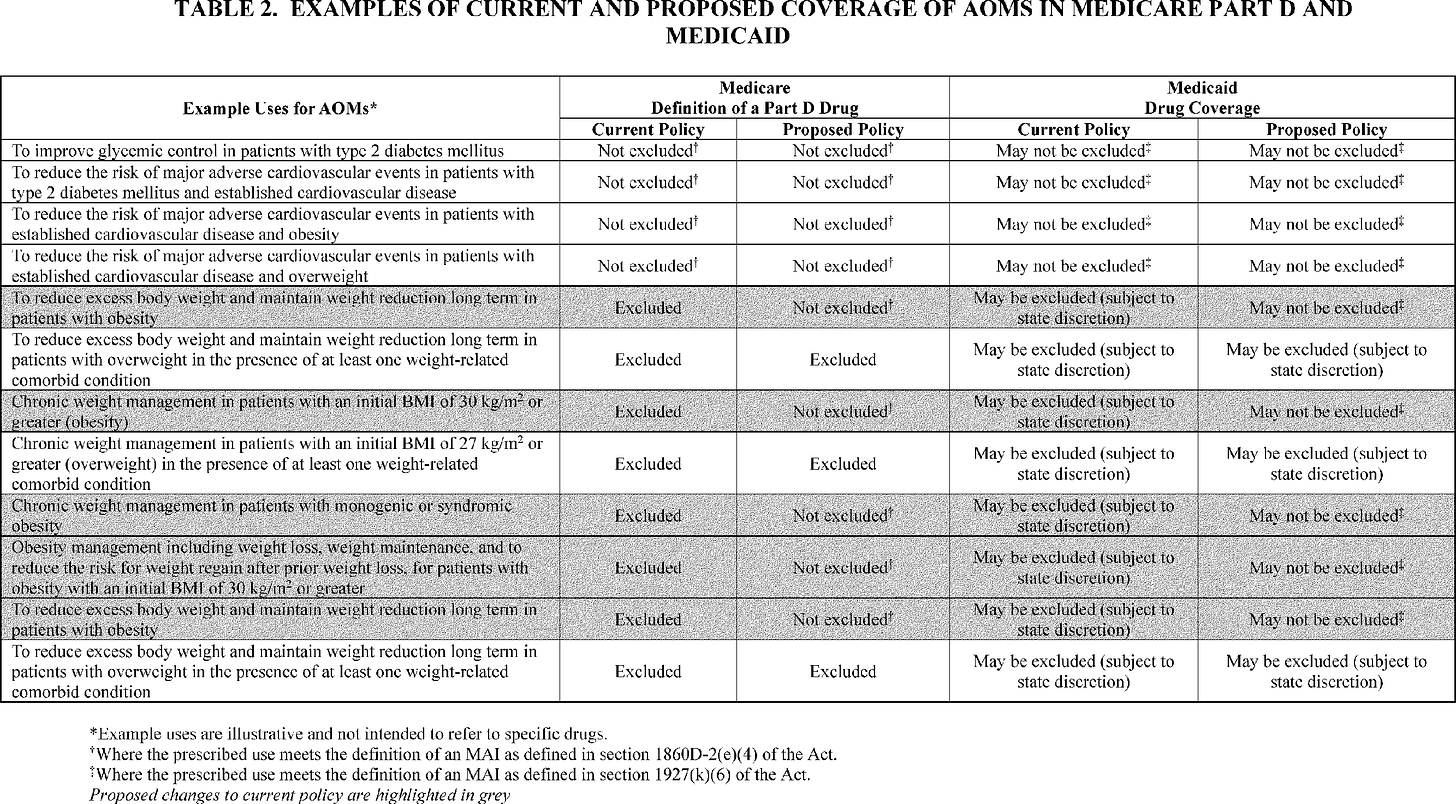
Given the changes in how the medical community has come to regard obesity as a disease since the start of the Part D program, CMS believes that its longstanding interpretation of the reference in section 1927(d)(2) of the Act to “[a]gents when used for . . . weight loss” as including AOMs when used for weight loss or chronic weight management regardless of whether the AOMs were used to treat obesity reflects an outdated medical understanding, and that it would be more consistent with current medical views to propose to reinterpret the phrase “[a]gents when used for . . . weight loss” to exclude AOMs when used for the treatment of obesity. As a result of this proposed reinterpretation, AOMs— when used for weight loss or chronic weight management for the treatment of obesity—would no longer be excluded from Part D coverage based on section 1860D-2(e)(2) of the Act, which prohibits Part D coverage of “drugs or classes of drugs. . .which may be excluded from coverage or otherwise restricted under section 1927(d)(2).” In addition, CMS would no longer consider AOMs when used for weight loss or chronic weight management for the treatment of obesity to be excluded from the definition of Part D drug at § 423.100, which at paragraph (2)(ii) excludes drugs that may be excluded from Medicaid coverage under section 1927(d)(2). Our proposal is not contingent on the underlying etiology of obesity (for example, due to unspecified causes or specified causes such as drug-induced obesity or obesity due to specific genetic variants or syndromes) and would encompass any drugs that are indicated for weight loss or chronic weight management for the treatment of obesity. In table 2., we provide examples to illustrate the effect of our proposal on AOM coverage in Medicare Part D.
Now don’t get confused with overweight. People “with overweight” (their words, not mine) are excluded, because “overweight is not recognized as a disease”.
YET.
But I mean, can you feel the discrimination…the exclusion??? Do you hear the judgement and the assumptions about people with just overweight? I hope someone catches this and fixes the disparity. I’m pretty sure we need another reinterpretation already.
We are not proposing to reinterpret the statutory exclusion of “[a]gents when used for . . . weight loss” in section 1927(d)(2) of the Act to permit Part D coverage of AOMs when used for weight loss or chronic weight management in individuals with overweight, even if such individuals have weight-related comorbid conditions. We are not proposing such a change in interpretation because, unlike obesity, overweight is not recognized as a disease. The FDA-approved indications for most AOMs used for weight loss or chronic weight management specify that individuals with overweight must also have weight-related conditions, but there is no such requirement for the presence of comorbid conditions in individuals with obesity. We believe this supports recognizing obesity as a distinct disease. Our proposal to limit the reinterpretation to AOMs used for weight loss or weight management for the treatment of obesity is based on the distinction between obesity as a disease and overweight, which is not recognized as a disease, but may occur in combination with other conditions that are weight related. As we have discussed, some AOMs are FDA-approved to improve glycemic control in patients with type 2 diabetes and reduce major cardiovascular events in adults with established cardiovascular disease (in adults with type 2 diabetes, obesity, or overweight), independent of the indication for weight loss or chronic weight management. AOMs that have received FDA approval for these uses have demonstrated effectiveness in these conditions (which are common weight-related conditions) independent of weight loss. Therefore, we believe that for individuals with overweight, the current policy for coverage under Part D should be maintained to permit coverage of an AOM when the AOM is used for a weight-related condition for which the AOM has demonstrated effectiveness independent of weight loss and is an MAI. By contrast, in obesity, we consider weight loss to be the mechanism for reducing excess adiposity and mitigating its accompanying hormonal and metabolic dysregulation.
Luckily, they are aware of this blatant discrimination against people with overweight and invite comments about the reinterpretation.
pssst….I wonder if they’re trying to get the “just overweights” included…🤔
We acknowledge, however, that by limiting our proposed reinterpretation, we could create a perverse incentive for some individuals with overweight to gain additional weight in order to meet criteria for obesity. We solicit comment on our proposed reinterpretation, including our underlying assumptions and the decision not to extend our reinterpretation of the statutory exclusion to provide that individuals with overweight and at least one weight-related comorbidity could receive coverage of AOMs for weight loss or chronic weight management under Part D.
Ok, here’s the skinny…😉
If you are just an overweight, as long as you have another condition for which these murder shots medications are indicated, you’ll still be able to get your doctor to prescribe them even if our reinterpretation doesn’t get amended you might have a weight related comorbidity that will qualify you.
In general, Part D sponsors must cover formulary drugs for all FDA-approved indications that are not excluded from Part D coverage.[] Most available AOMs are also indicated for use in individuals with overweight with weight-related comorbid conditions. A weight-related comorbid condition might include, for example, hypertension, type 2 diabetes, dyslipidemia, sleep apnea, or cardiovascular disease. As stated previously, some available AOMs contain the same active ingredients approved by the FDA to improve glycemic control in patients with type 2 diabetes and reduce major cardiovascular events in adults with established cardiovascular disease and type 2 diabetes, and one AOM has received FDA approval to reduce the risk of major adverse cardiovascular events in non-diabetic adults with established cardiovascular disease and either obesity or overweight. Therefore, individuals with type 2 diabetes or established cardiovascular disease (with type 2 diabetes, obesity, or overweight) are already eligible for AOM coverage under current policy because these FDA-approved indications are distinct from the indication of weight loss or chronic weight management.
And the obeses will qualify, regardless. Phew.
👇Ozempi-Hack👇
Get a Telemed appointment and just lie about your weight.
Or just put some heavy shit in your pockets and get your golden
Ozempi-Ticket-Obese Label.
Should our reinterpretation be finalized as proposed, individuals with obesity would be eligible for AOM coverage covered regardless of weight-related comorbid conditions. In comparison, AOMs used for weight loss or chronic weight management in individuals with overweight, who do not have another condition that is an MAI for the AOM, would continue to be excluded from the definition of a Part D drug and would not be coverable under Part D. In other words, Part D sponsors would continue to exclude drugs with FDA-approved indications of weight loss or chronic weight management in individuals with overweight with weight-related comorbidities from Part D coverage, unless the individual has another condition that is an MAI for the AOM. See examples in table 2 illustrating the effect of our proposal as it relates to AOM coverage for individuals with overweight. Consistent with current guidance, CMS expects Part D sponsors to consistently utilize PA for drugs with the highest likelihood of non-Part D covered uses, including when there is a high likelihood that a drug's medical use is excluded from Part D coverage.[]
Here’s the exciting summary of the “medical consensus”🤗
5. Summary
In summary, due to changes in the prevailing medical consensus towards recognizing obesity as a disease, we are re-evaluating Part D coverage of AOMs for Medicare beneficiaries with obesity who do not have another condition for which an AOM is indicated and for whom the prescribed use would be otherwise coverable under Part D. As a result of our proposed reinterpretation of the phrase “[a]gents when used for . . . weight loss” in section 1927(d)(2) of the Act, AOMs that are used for treating obesity and that otherwise meet the definition of Part D drug at § 423.100 would no longer be excluded from Part D coverage pursuant to the exclusion in paragraph (2)(ii) of that definition for drugs that may be excluded from Medicaid coverage under section 1927(d)(2) of the Act. Our proposed reinterpretation would also apply to Medicaid such that state Medicaid programs would no longer have the discretion to exclude AOMs from Medicaid drug coverage as “[a]gents when used for . . . weight loss” when used for weight loss or weight management for the treatment of obesity. If our reinterpretation is finalized as proposed, states that are not already covering AOMs for weight loss or weight management would be required to do so to treat obesity in Medicaid enrollees with obesity. AOMs, when used for weight loss or chronic weight management in individuals who do not have obesity, would continue to be excluded from the definition of Part D drug, and may be excluded at state option from coverage by state Medicaid programs, unless the AOM is being used for a condition other than weight loss or chronic weight management for which such use would be covered as an MAI as defined in section 1927(k)(6) of the Act.
And here’s a helpful table using a template from a 1988 elementary school worksheet:
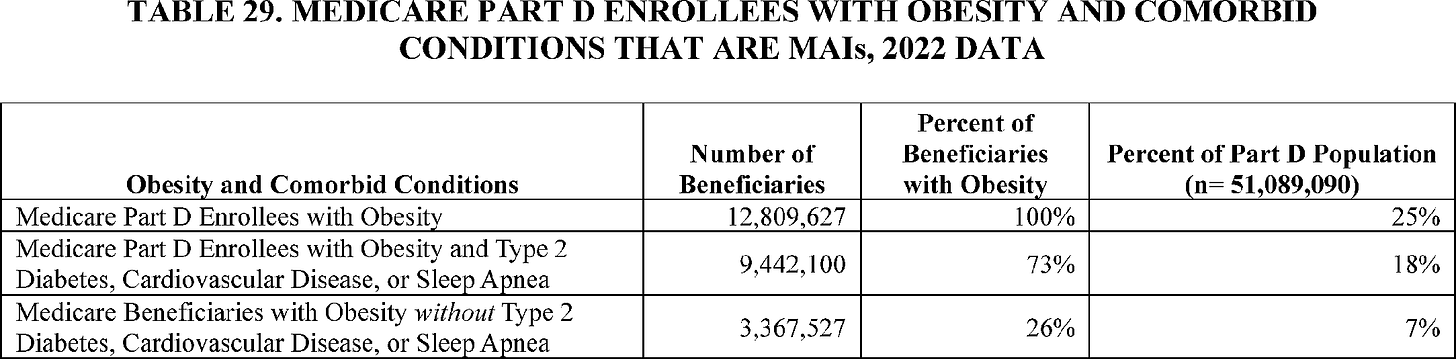
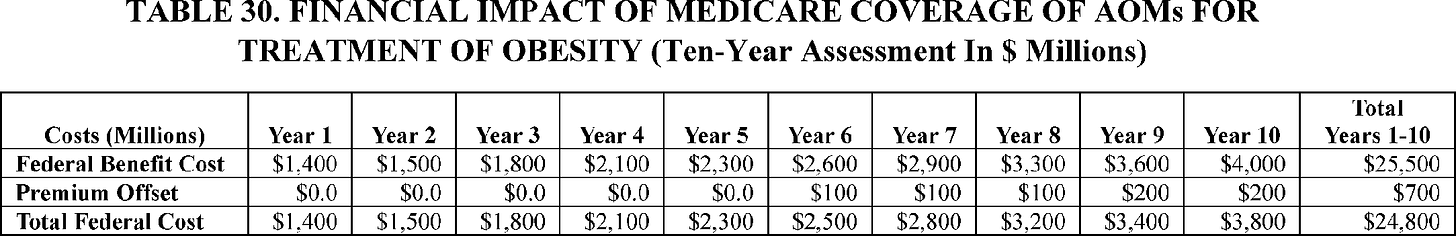
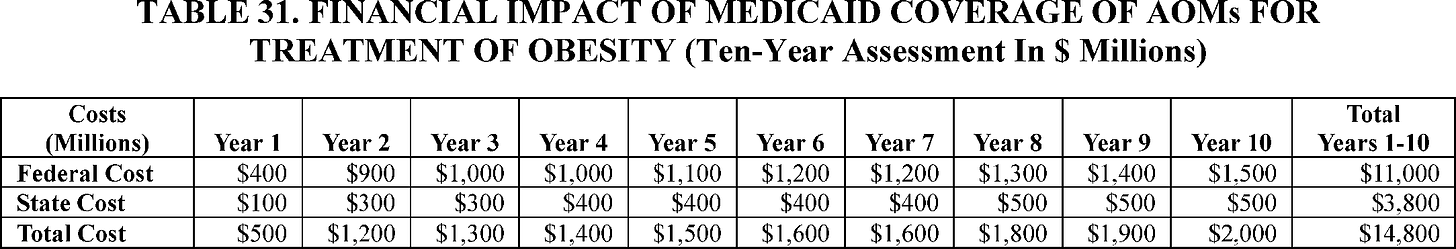
And now the financial breakdown. But please know that this might “possibly” be a “significant underestimate”. Just throwing that in there so that they can be sure to remind you about how up front they were with their underestimation when it costs a gazillion billion dollars. I think they might be moving at the speed of Science™, so all bets are off fuckers.
It is possible that our estimates significantly underestimate the impact of our proposal. These estimates are sensitive to the utilization rate, which has a high degree of uncertainty. We factored in an estimated discontinuation rate based on published literature, but discontinuation rates and duration of therapy before treatment is discontinued vary in the literature.[] Our assumption may not fully reflect patients who discontinue but subsequently resume treatment with AOMs.
The experts are here and they’ve crunched the numbers fools…and their estimations are definitely maybe going to be potentially higher or possibly lower than sales pitched projected.
Costs may be significantly higher or lower than projected. Our estimates relied on assumptions about rates of obesity and other conditions in the Medicaid population since T-MSIS does not contain complete diagnosis-level data. It is possible that a larger proportion of the Medicaid population has obesity without other conditions since the Medicaid population is younger than the Medicare population and therefore may not yet have developed other conditions that are coverable under the current policy.
Welp, that’s it for this post. The Federal Register sure was a blast.
Stay tuned, it’s FedReg Fuckery Season!






Oh good! Now when the famine happens, the people taking these stomach-paralyzing Gila monster shots won’t be competing with me for food.
I suppose if you were only overweight, you could put on a bigger frock and insist that you identify as a transing-to-obese person.
Oddly, over here on Airstrip One, they're doing something similar, although not with Ozempic but with some similar product I hadn't heard of. There's less admin, of course, since with the NHS, Stealth Depop (sometimes still quaintly referred to as 'healthcare') is free at the point of use, but isn't it weird that, whether it's assisted suicide or covert suicide (Ozempicide?) these things now happen in different countries at the same time. Almost as if ... oh, never mind.